The first thing to know is that “heavy metal” is something of a misnomer. Scientists disagree about how to define the term and its utility. In theory, a heavy metal should be a metallic element that has a relatively high density or weight. But in practice, ‘heavy metal’ is often used to refer to a subset of metals and metalloids with harmful effects on human health. Yet multiple essential nutrients (e.g. iron, copper, and zinc) could be considered part of the same group by periodic property, and literal heaviness dictates nothing inherent about a material’s toxicity.
“I prefer to use the term elements,” says Manish Arora, a professor and vice chairman of environmental medicine and climate science at the Mount Sinai School of Medicine in New York City. Arora considers elements in three categories: those that are essential for our physiology in small quantities, those that are neither needed nor necessarily harmful, and those that are toxic without offering any health benefits.
There’s additional complexity within those categorizations. For instance even some essential elements (like iron) can become harmful in excess. But when people talk about “heavy metals” they’re often thinking of the group number three–including things like lead, arsenic, cadmium, and mercury, says Kelly Bakulski, an associate professor of epidemiology at the University of Michigan, where she studies the influence of environment and genetics on neurological disorders.
What are the health risks?
Exposure to each of these elements has been linked to varied health harms, with increased exposure carrying increased risk. Arsenic, for instance, is a known carcinogen, associated with bladder and lung cancers, says Bakulski. It’s also known to cause skin lesions, raise risk of heart problems, and is associated with developmental disorders in childhood, according to the World Health Organization. Cadmium, too, is a notorious carcinogen. Mercury is linked with cognitive problems such as insomnia, tremors, and memory loss. Lead exposure brings a litany of neurological and systemic risks. In utero and in children, it can lead to lifetime cognitive impairments and behavioral difficulties. In adults, lead exposure can cause vascular problems, says Bakulski, and early research from her lab indicates it may play a role in dementia and Alzheimer’s development as well.
[ Related: What science actually says about seed oils ]
Route of exposure can change the health risk and severity of effects of an environmental exposure, says Arora. Even something like manganese, which is an essential nutrient in small, ingested quantities, can be dangerous when inhaled. Welders who don’t wear the proper safety equipment or work in unsafe conditions, he notes, can develop manganism, a disorder with symptoms similar to Parkinson’s. And combinations of elements can exacerbate risk. Lead and excess manganese exposure together is more toxic than either element alone, he adds.
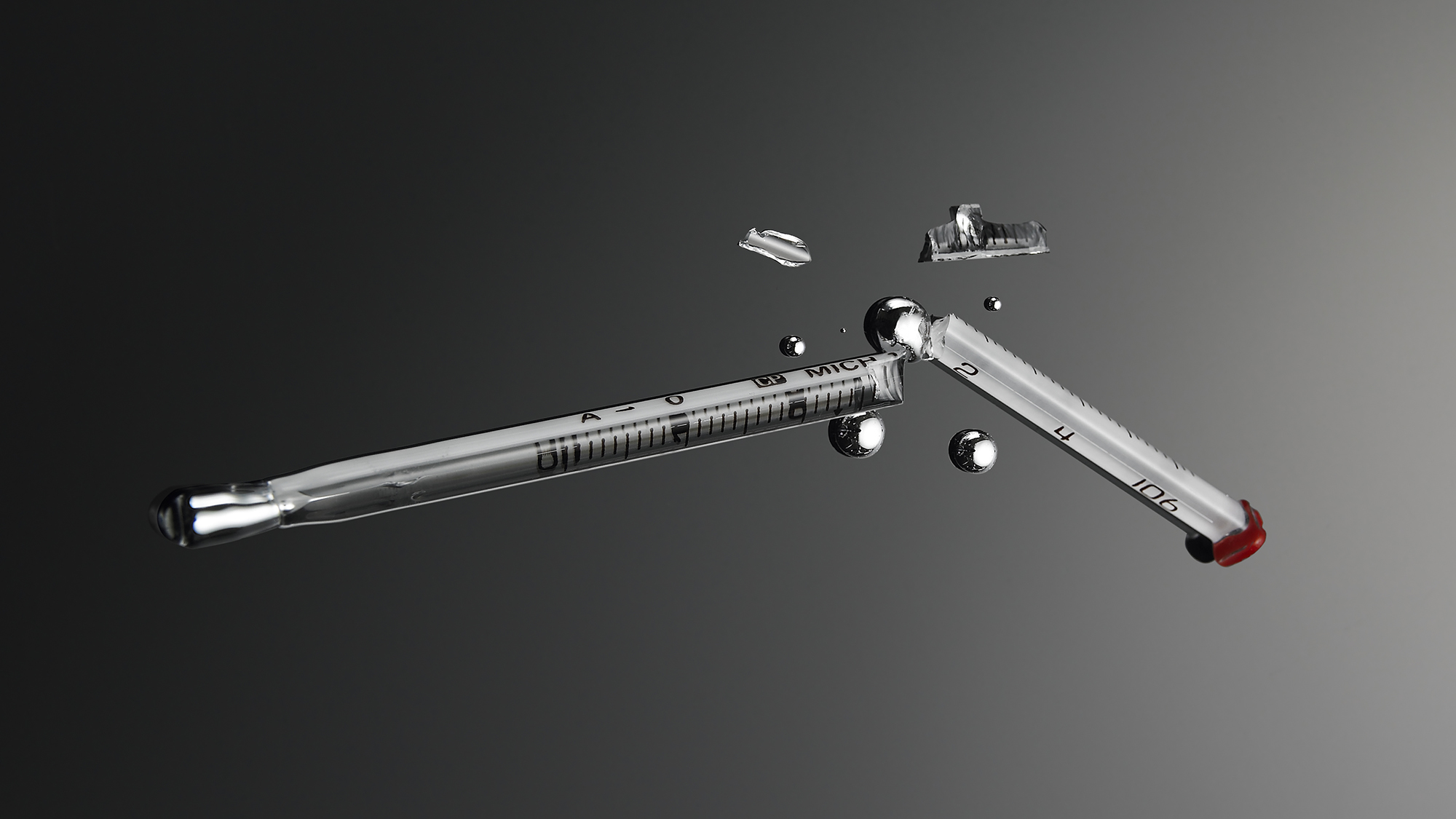
Finally, chemical form is a key factor in risk. Some compounds containing these elements are toxic, while others are benign in small doses, as they’re more readily excreted. An example of this would be ethylmercury, which is a mercury-containing compound that’s broken down and passed much quicker than methylmercury, the compound that bioaccumulates in seafood and human bodies. The thimerosal preservative present in some vaccines is metabolized into ethylmercury, and so does not carry the same risk as toxic methylmercury.
What are common sources of ‘heavy metals’? How are we exposed?
Each of these elements is, broadly speaking, rare or diffuse in the natural environment. But in many cases, human activity and pollution has made environmental exposure more common. And, in certain places, geology and geography mean these compounds exist in higher background concentrations to begin with, says Bukalski.
Humans are in contact with a mix of pollutants in our day-to-day lives, says Arora. “We encounter a soup of exposures. Nobody gets exposed to just one thing,” he adds. You might inhale, ingest, or absorb a variety of toxic elements via the air, water, food, smoke, or a tainted skincare product.
For decades, lead was added to gasoline, distributing lead particles into the air and soil through car exhaust. Now industrial pollution is the leading source of lead air emissions. In old houses, dust usually contains lead because of the layers of lead paint on the walls. Flint, Michigan became the poster city for the all-too-common problem of lead leaching into drinking water via a devastating combination of water chemistry and old infrastructure. Certain foods can be a significant dietary source of mercury, cadmium, or arsenic (seafood for mercury, rice and other grains for the latter two). Arsenic can also be present in drinking water, depending on region. Tobacco smoke–both first- and second-hand–is a significant source of cadmium exposure, says Bakulski, as tobacco sequesters cadmium from the soil as it grows.
What about vaccines?
One common misconception is that vaccines are a source of ‘heavy metal’ exposure, and carry toxic health risks–especially for infants and children. This idea dates back to the 1998 publication of a now retracted and thoroughly debunked study of 12 children that purported to find a link between the measles, mumps, and rubella (MMR) vaccine and autism. The study pinpointed thimerosal, a mercury-containing preservative in the vaccine, as the allegedly dangerous component. Yet investigation into the research found that results had been falsified and that the study was the product of scientific fraud. Andrew Wakefield, the researcher behind the faulty work, lost his medical license in the debacle–in part, over revelations that he had been paid a considerable sum of undeclared money by a lawyer seeking to generate evidence of a link between the vaccine and autism for a legal case.
[ Related: How to talk to your ‘skeptic’ family about science misinformation ]
More than a dozen subsequent studies of vaccines and, specifically, thimerosal have found no link between the shots or the specific preservative and autism. Moreover, follow up research has found no evidence of any harm from thimerosal in vaccines, aside from rare allergic reactions. However, most vaccines used in recent decades no longer contain thimerosal because of manufacturing changes. None of the vaccine formulations recommended for children six years or younger contain thimerosal, since 1999, out of an abundance of caution, and to reduce potential childhood mercury exposure levels, in all forms.
“Vaccines are an incredible public health advancement. They’ve saved millions of lives,” says Bakulski. “This question [of vaccines and autism] has been rigorously investigated many, many times in cohorts of millions of participants with decades of follow-up. All have shown no association.”
“So much research has been done on vaccines and autism spectrum disorder, and we just don’t see that link at a population level,” says Arora. “None of the research I have seen convinces me there is any link.”
But do ‘heavy metals’ cause autism?
Vaccines are not associated with autism, according to the best available scientific evidence. However, there is some emerging evidence to indicate a link between toxic elements and autism spectrum disorder.
Autism spectrum disorder is a neurological and developmental difference that impacts how people communicate, learn, and act. People with autism display a wide range of symptoms and severity (hence “spectrum disorder”), but it’s often characterized by repetitive behavioral patterns and interests, and social difficulties. It’s complicated, and no single factor “causes” it, says Bakulski. It’s the result of an interplay between genetic and environmental factors, she says. As the current line of thought goes, some susceptibility is compounded or triggered by external conditions. For instance, extensive research suggests that exposure to air pollution at key timepoints during fetal development or in early life is associated with an increased change of an autism diagnosis.
Both Bakulski and Arora have conducted studies that found associations between toxic element exposure in early life and autism spectrum disorders. In research published this past July, Bakilski noted a significant connection between cadmium exposure in the first and second trimester in utero and an increased risk of developing autism.
Across multiple studies, Arora has documented links between toxic metal uptake and autism spectrum disorders. In twin and sibling studies, he’s found that people who go on to develop autism seem to have some vulnerability in their metal metabolism that makes them more likely to absorb toxic elements from their environment at critical stages of growth. As leader of the private company, Linus Biotechnology, he’s applying these findings to develop a biomarker test that uses a strand of hair to compile a time-series of elemental exposures and rule out whether a child is likely to develop autism, with the intent of making early diagnosis, and thus early treatment, more accessible.
But there is one big caveat to all of this: Just because pollution and toxic element exposure seem to be associated with autism, does not mean that treating metal exposure treats autism.
Can chelation therapy treat autism?
Chronic and acute poisoning with toxic elements like arsenic, uranium, mercury, and lead is sometimes treated with chelation therapy. Chelation uses compounds that bind toxic elements and helps people excrete these materials, which would otherwise continue to bioaccumulate, from their bodies.
Despite a proliferation of claims, there is no evidence that chelation therapy treats autism, says Stephen James, a researcher at the Southwest Autism Research and Resource Center in Phoenix, Arizona. In a 2015 review article, he and his colleagues reviewed the available research on chelation as an autism treatment. Only one of the 10 studies they were able to find met the criteria of a randomised trial, it still failed to include a proper placebo, and the chelation treatment showed no significant effect on autism spectrum disorder symptoms.
The logic behind chelation as an autism treatment is flawed, in part because the relationship between environmental exposures and autism development is so time-dependent, says Bakulski. There are windows in utero and early life where pollution exposure or metal metabolism are most important, long before autism itself is diagnosable. During these phases, the environment shapes the course of development. After progress has been made down a certain path, it cannot be unmade. Even if these developmental divergences are, in part, the result of toxic elements, removing those elements from the body later on will not undo the physiological or neurological shifts that have already taken place.
“There is absolutely no evidence to suggest that, even if individuals with autism have higher levels of heavy metals, that chelation therapy would reverse autism symptoms,” says James.
And chelation should not be undertaken lightly. It can be a dangerous treatment and should only be administered in approved cases under medical supervision, as binding agents can collect essential nutrients as well as toxic elements. In some cases, chelation can cause organ damage and other severe side effects. In 2005 a five-year-old autistic child died of a heart attack as a result of chelation therapy. The cardiac arrest was caused by hypocalcaemia– or a dearth of calcium, which is critical for maintaining heart function and rhythm.
How can you protect yourself?
In the U.S. and many places around the world, public health policies and environmental regulations have already greatly reduced our day-to-day risk of exposures to toxic elements. The Clean Air Act, drinking water standards, workplace safety requirements, and FDA monitoring for contamination in the food supply have been instrumental in minimizing pollution exposure, says Bakulski. The best way to make additional strides towards a cleaner, healthier, less harmful environment is to strengthen these regulations, she adds–in direct contrast with calls to dismantle federal regulatory agencies or weaken their capacity for oversight.
Though an individual level, there are some things you can do. Avoiding tobacco smoke is a major way to reduce your exposure risk, says Bakulski. Eating a balanced, nutritious diet is another key factor. Many toxic elements cause problems by replacing necessary elements in our bodies’ complex network of chemical reactions. If you eat enough of your essential nutrients, then enzymes are less likely to inadvertently bind to a toxic element than to the intended essential elements. Additionally, aiming for variety and avoiding overconsumption of any single food minimizes your risk of taking in high levels of any particular unwanted element.
Both ‘heavy metals’ and misinformation are widespread pollutants. Unfortunately, cleaning up the information environment has proved perhaps more difficult than cleaning up the actual environment. We know how to minimize lead contamination in our homes and pipes, for instance, but ideas can prove intractable. Despite decades of research debunking common misconceptions about vaccines, toxic elements, and autism, harmful misunderstandings persist. To understand the truth, it’s important to look beyond the surface, and dig into the science.
This story is part of Popular Science’s Ask Us Anything series, where we answer your most outlandish, mind-burning questions, from the ordinary to the off-the-wall. Have something you’ve always wanted to know? Ask us.