This story was supported by the journalism nonprofit the Economic Hardship Reporting Project.
In early 2020 I developed a disabling case of long COVID, which sent me on a never-ending search for adequate care. Three of the most prominent long COVID clinics in Los Angeles turned me away because I wasn’t able to obtain a test for the virus when I fell ill, an experience shared by many patients who were infected early in the pandemic, when resources were still nonexistent or scarce. But in late 2021 I was able to make an appointment at Keck Medicine of USC’s COVID Recovery Clinic. I was hopeful that I would be seen by a doctor with experience treating complex chronic illnesses since some infectious diseases such as SARS, mono, and Lyme are known to result in long-term conditions.
The same December, I was seen by a family medicine physician and physical therapist. The clinicians met with me for an hour and later referred me to a neurologist—who I wouldn’t be able to see for four months—and prescribed me an antidepressant that the physician said may help my headaches. I was told to follow up in one to three months despite the severe side effects that fractionated my work hours, made my hobbies of rock climbing and running impossible, and altered every aspect of my life. Before my appointment wrapped, I asked about possible treatments based on up-to-date long COVID research, but was turned down because of my symptom profile. I left defeated and hopeless.
My experience is not unique. This summer, the US Census Bureau reported that close to 16 million American adults are living with long COVID, a debilitating condition that lasts at least four weeks beyond an initial coronavirus infection and affects multiple organ systems. It has been observed in all age groups, and has placed stress on the US healthcare model that relies on short doctor’s visits. Even though high-demand clinics, sometimes called post-COVID care centers, now offer services for the illness, many fail the very patients they have set out to help. Long COVID patients share anecdotes about how the clinics they are admitted to often turn a blind eye to the gravity of their needs and fail to incorporate knowledge learned from myalgic encephalomyelitis, or ME, and other infection-associated illnesses.
[Related: Long COVID can manifest in dozens of ways]
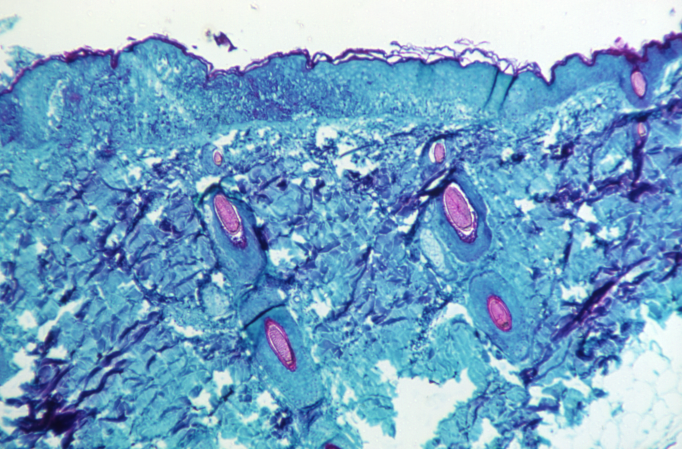
ME, which is sometimes called chronic fatigue syndrome, is a disease that often appears in the wake of an infection. In a small observational study recently done on long COVID patients, nearly half met the diagnostic criteria for ME, including substantial impairment in both physical and cognitive function alongside post-exertional malaise—a flare-up of symptoms that typically appear a day after cognitive or physical exertion—and fitful sleep. It also can cover cognitive impairment or orthostatic intolerance, meaning the inability to remain upright without extreme dizziness and other symptoms. While most people living with long COVID or ME developed their illness after infection, a very rare group of people are known as vaccine-injured, meaning they developed similar symptoms after getting the coronavirus jabs.
Clinics informed by ME offer insight into managing long COVID with treatment and education, providing a rubric for how other recovery centers could operate. Their approach also exposes the structural neglect of complex chronic illnesses in the US.
Lucinda Bateman, founder and medical director of the Bateman Horne Center in Salt Lake City, is one of a small number of ME specialists in the county. She has been treating and researching the illness for more than three decades. “I can tell you from our close assessments that many people with long COVID become severe enough and chronic enough to meet these criteria [for ME/CFS],” she says. “So I would consider them SARS-CoV-2 induced ME/CFS.”
Hard-to-find care
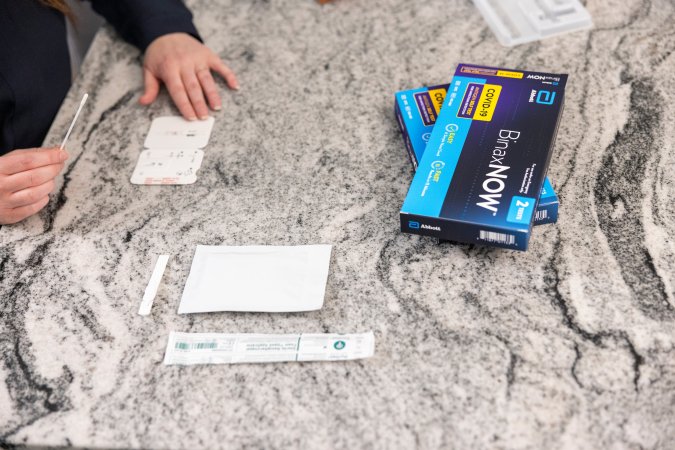
Inaccessibility is one of the most prominent barriers to post-COVID clinics. Most require a positive test and a referral from a patient’s primary care physician. With nearly 26 million people uninsured in the US and many more who are inadequately covered, seeing a primary care physician can be a financial burden, especially if patients are chronically ill and unable to work.
Distance is another factor. According to the COVID-19 Longhauler Advocacy Project, the US has more than 400 long COVID clinics and rehabilitation centers, but few exist in rural locations and only around a dozen focus on pediatric long COVID patients. Traveling long distances is an enormous burden on long COVID patients, who may be bed- or housebound. What’s more, many physicians continue to consider their patients’ symptoms (and sometimes even their colleagues’ symptoms) to be psychosomatic, or the result of stress or anxiety, which can make getting a referral to a clinic challenging.
If a patient is able to clear these barriers despite their extreme fatigue, cognitive impairment, and cluster of more than 100 other possible symptoms, they typically encounter months-long waiting lists to be admitted to clinics.
Desireé Parker, a 39-year-old from Pennsylvania, had to wait almost half of a year to be seen by the University of Pittsburgh Medical Center’s Post-COVID Recovery Clinic. When she had her first appointment this summer, she says the clinic ordered some lab work and gave her basic informational handouts. “It was just very generic,” she recounts from her experience. “It was like a packet of internet sources … I expected a lot more after waiting patiently for five months.”
Beyond these forms of inaccessibility, patients say some doctors at long COVID clinics aren’t aware of recent studies of the disease, which link it to markers of complex chronic illnesses like microclots and autoimmune responses, reactivated viruses like Epstein-Barr, and common concurrent diagnoses like postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome (MCAS), and others.
One of the least-acknowledged, but most-critical-to-address questions of long COVID is how it overlaps with ME. Before the COVID pandemic began, as many as 2.5 million Americans were already living with ME. Because the disorder has been stigmatized and underfunded for decades, few physicians are are able to diagnose and treat it. In fact, less than one-third of medical school curricula in the US include education about ME.
Beyond inaccessibility, patients say some doctors at long COVID clinics aren’t aware of recent studies of the disease, which link it to markers of complex chronic illnesses.
These systemic issues are now having a resounding impact on people seeking comprehensive long COVID care. Sara, a 30 year-old who wished to omit her last name, says that in the fall of 2021, when she had a virtual appointment with MedStar Health COVID Recovery Program in Maryland, her doctor told her that her symptoms were due to untreated anxiety and depression—a common experience for patients with chronic illness, particularly women and people of color. She worked with a lawyer to attempt to get the psychosomatic note off her record because she said it might put the private long-term disability insurance that she was applying for in jeopardy.
“At best, he was ignorant,” Sara says about her doctor at the clinic. “And at worst, he was actively being harmful.” Her concerns inspire a larger question of how post-COVID care centers are screening patients for the complex list of markers for the disease. When I reached out to a representative of MedStar to ask if their clinic believed long COVID and its concurrent diagnoses were psychosomatic despite vast scientific literature showing the disease affecting multiple organ systems, I didn’t receive a response. Sara left MedStar’s clinic and later went to George Washington Medical Faculty Associates COVID-19 Recovery Clinic in the D.C. metro area. There she had a promising initial visit where they diagnosed her with dysautonomia—an umbrella term for disorders of the autonomic nervous system including syndromes like POTS—and referred her to a cardiologist for further care. But the facility closed this summer and transitioned their patients to primary care providers, an emerging trend in the US and abroad.
Outdated therapies
Because so many physicians are uninformed about ME, some at long COVID clinics prescribe therapies that have been proven to be harmful to patients who experience post-exertional malaise (PEM). Graded exercise therapy (GET)—a controversial form of physical therapy for ME and long COVID which slowly increases exercise over time— worsens patients’ symptoms who experience PEM. “Graded exercise therapy implies that you can exercise yourself into fitness and resolve the illness,” Bateman says. “When in reality, that’s not the case.”
Jordan, a 23-year-old who wished to omit his last name, says he was referred for pulmonary rehabilitation after two visits to Houston Methodist’s COVID-19 Recovery Clinic in the spring of 2022. He followed a program of increased aerobic exercise resembling GET for about a month. “24 hours after I finished each session I’d get a flare-up of symptoms,” he says.
Jordan says he has been living with long COVID symptoms since getting his second COVID-19 vaccination dose in May 2021. Before that, he had two prior SARS-CoV-2 infections. Though there are few studies on post-vaccine side effects, some immunologists believe it may provide clues on the biology of long COVID.
His symptoms got progressively worse as he followed the GET-like program, leading to lightheadedness and “burning” headaches. When Jordan mentioned this to a nurse practitioner at the Houston Methodist clinic, he says he was told to continue exercising, do cognitive behavioral therapy, and come back in six months.
A spokesperson for Houston Methodist wrote to me that they do not prescribe GET at their post-COVID clinic, but that if a patient at the clinic requires pulmonary rehabilitation a respiratory therapist may recommend a “gradual exercise regimen” based on that individual’s needs. Jordan says his therapy included an increase in the length of the time of the exercises, which is a feature of GET. I asked by email if and how the clinic—or any medical professionals the clinic refers to—prescribes the therapy to patients with PEM, but didn’t receive a response.

Jordan left the clinic in summer and was recently admitted to Baylor’s Post COVID Care Clinic in Texas after a five-month wait. He says he feels heard at the clinic and that his primary provider is much better informed about ME and its ties to long COVID.
“The issue is that for most clinicians the disease is incredibly complex,” says Jaime Seltzer, the director of scientific and medical outreach at the advocacy group #MEAction. Clinicians who are faced with this level of complexity, she says, may turn to treatments like GET because they are based on simple hypotheses.
The most prominent study used to employ GET is the 2004-2011 PACE Trial, which has been debunked as an outdated standard of care in a recent ME consensus recommendation written by Bateman and 22 other co-authors. The CDC even removed recommendations for GET from its website in 2017. The therapy is also not recommended for people with ME by the National Institute for Health and Care Excellence, which offers guidelines for health and care in England, nor is it recommended for long COVID patients who experience PEM by the World Health Organization.
“There is a lot you can do for ME/CFS,” Seltzer says. “There’s no cure, but that’s not the same thing as saying it cannot be managed.” She points out that many people with ME have grown frustrated with the narrative that long COVID is a new and mysterious illness, and says that it perpetuates an excuse for clinicians to not be blamed for failing to help. “It is absurd that they are turning away good information because of stigma.”
Akiko Iwasaki, an immunologist at Yale School of Medicine and a leading long COVID researcher, agrees with Seltzer: Had there been more research and funding devoted to studying ME, she says, we would have been much better prepared to deal with long COVID. “I’m hoping that any insights we gain from long COVID will also apply to [ME].”
Managing ME
In preliminary research posted online this August, Iwasaki and her colleagues found altered immune cell activity, blood abnormalities, low cortisol levels, and signs of reactivated Epstein-Barr virus in long COVID patients. She says that their findings warrant an immediate need for randomized clinical trials to target these syndromes. Long COVID clinics would be a natural place for them to begin. “As a scientist I’d like to know all the pieces of the puzzle first,” she explains, “But we don’t have that luxury, we have to start trialing to find something that works now.”
At some point, long COVID will become enough of an issue that it will demand change, but ME specialist Lucinda Bateman worries about how many people will have to suffer until then.
Iwasaki’s top candidates for potential therapies to study include antivirals, like the drug Paxlovid, which will undergo its first clinical trial to alleviate inflammation and other long COVID symptoms in January. Early results from a widescale study on veterans found that the treatment with nirmatrelvir—one of the two pills used in the treatment—can slightly decrease the risk of long COVID if taken during the acute phase. Iwasaki also hopes to investigate other therapies that target the reactivated Epstein-Barr virus and inflammation associated with long COVID, as well as cortisol supplementation therapies.
But until more long COVID clinics begin testing potential therapies, Iwasaki says that at the very least there should be “open communication” between these clinics so that they can share insights about what works for patients and what doesn’t. Programs should standardize their training for physicians, too, which may be helped by the Biden administration’s proposed Centers of Excellence, so long as the model prioritizes infection-associated illnesses like ME.
Iwasaki underscores that each clinic should be set up so that patients can see many specialists in one visit. “That would be very helpful because people with long COVID often have brain fog that makes it very difficult to maneuver 12 different appointments,” she says.
One emerging model hoping to lead in this space is RTHM, Seltzer says. The new virtual long COVID clinic was co-founded by clinicians and researchers whose care is informed by their own patient experience with ME and other infection-associated illnesses. It sees patients virtually in five states, and targets ME, POTS, MCAS, and other conditions that often accompany long COVID. Seltzer is helping to shape the program’s educational resources.
Long COVID patients have begun visiting clinics and practices like RTHM that specialize in ME, even though the programs may be out of network with major health insurance carriers for some of their services. The nonprofit research advocacy group Solve M.E. shares a list of 17 doctors specializing in ME on their website; #MEAction has similarly compiled an international list of providers and allies. But many of these specialists are nearing retirement age at a time when their expertise is required by millions of survivors.
[Related: Getting COVID more than once might be even worse than we thought]
At Bateman’s ME clinic in Utah, she hired and trained two advanced practice clinicians to see long COVID patients, after she noticed a surge in need in late 2020. Like other medical experts I spoke with, she says the best way to address the growing need for ME and long COVID clinicians is to educate all healthcare workers about the illness. She also emphasizes that it’s necessary to put pressure on powerful agents like health insurance companies and academic institutions to recognize ME. “We need skilled chronic illness managers to coordinate the care of people with long COVID and other post-viral conditions,” she explains, far beyond those working in a few clinics.
In the meantime, Bateman recommends long COVID patients do the same thing she has been telling ME patients for years. “Become very well-informed yourself,” she says, advising individuals to read broadly about their own condition from ME non-profits, patient-led research groups, and papers written by ME specialists. “Secondly, work with a provider that you can communicate with and learn about long COVID together. It’s easier to train up a trusted doctor than to go searching for [ME specialists] when the numbers are still so low.”
At some point, long COVID will become enough of an issue that it will demand change, Bateman says, but she worries about how many people will have to suffer until then. “I’m hopeful that the response to long COVID will improve. But I would like to see it move more quickly and include all of the people with post-viral syndromes who are in need.”