COVID-19 is no longer a public health emergency in the US. The Biden administration’s deadline follows the World Health Organization’s announcement last week that removed COVID’s status as a global health crisis.
Infectious disease experts tell Popular Science that it’s an encouraging step and a sign that we are in a very different place than where we were in 2020. And while the recent decisions in no way mean the virus is gone—it’s expected to be endemic like the flu—access to COVID testing, treatments such as Paxlovid, and the vaccines have put the US in a position to coexist with it.
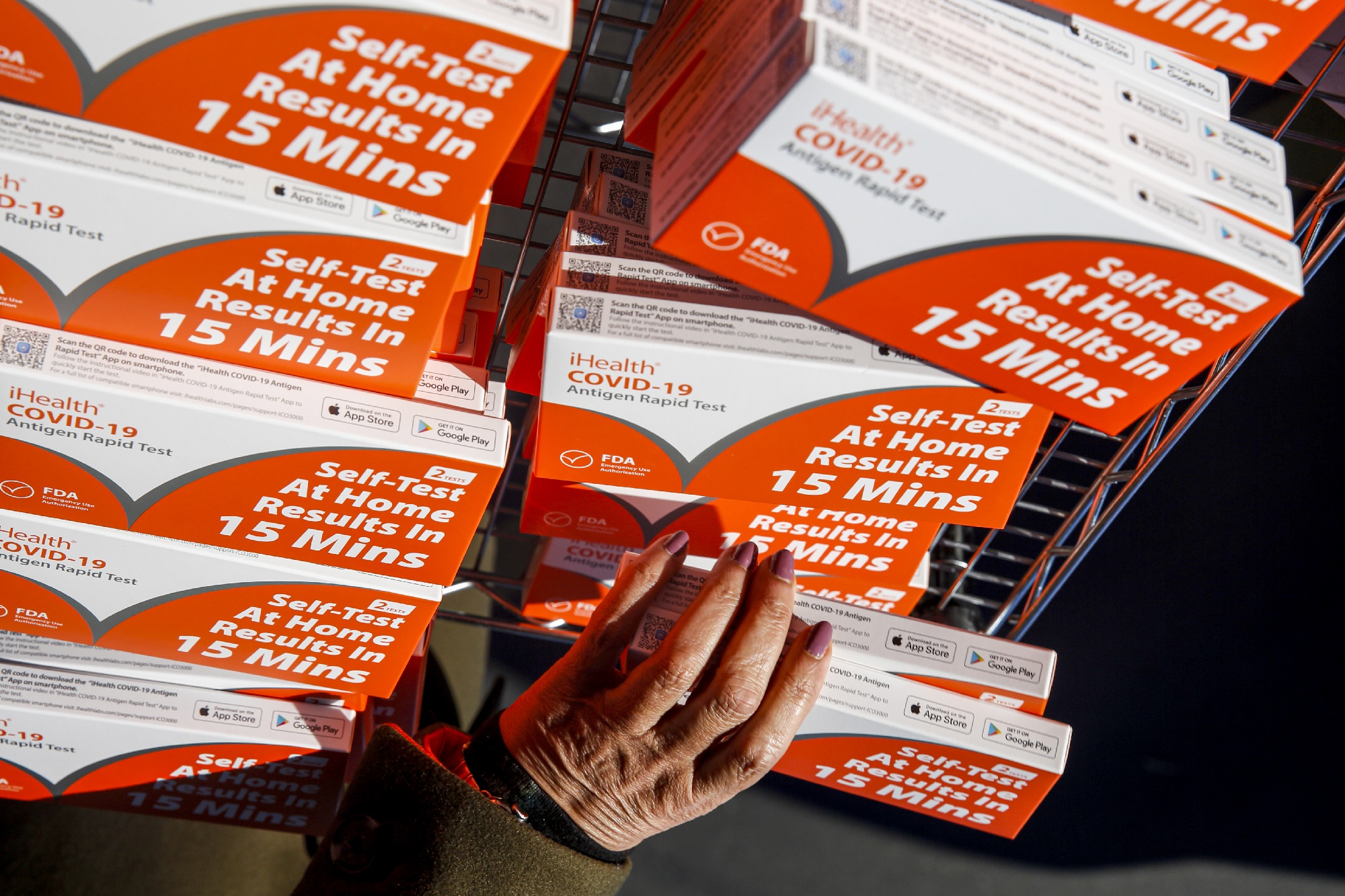
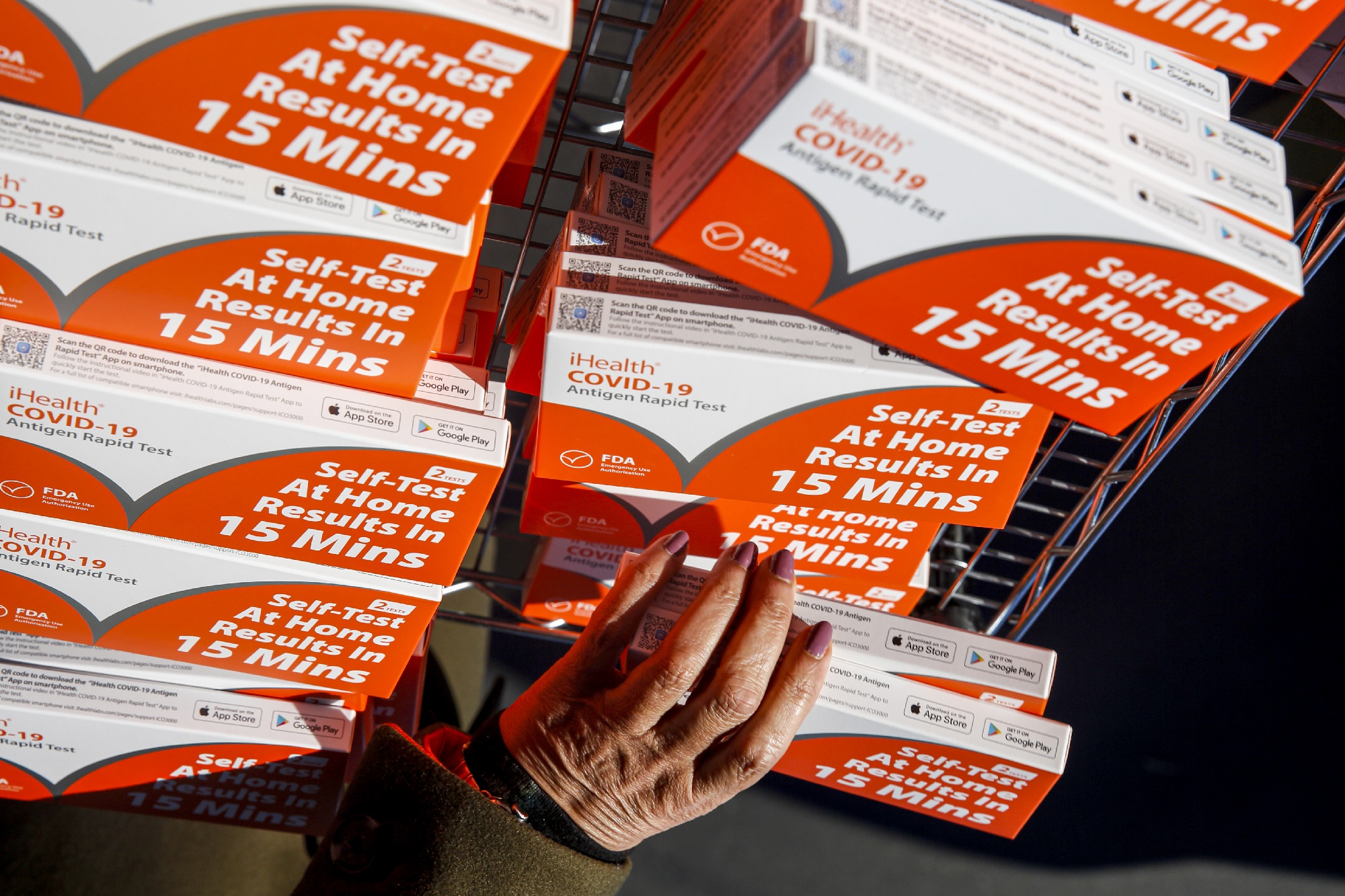
That said, managing your safety will come at a higher cost now. In one of the biggest changes from ending the federal emergency response, insurances are no longer required to cover the costs of COVID testing or reimburse people if they bought an over-the-counter home COVID-19 test. The federal government is also ending its free COVID-test program over the mail.
As the financial burden of testing shifts to families and individuals, knowing where and when to get tested will keep you protected as the country transitions into this new stage of the pandemic. “We’re still seeing up to 1,000 deaths a week in the US from COVID for people that are older and at risk,” warns Del DeHart, a medical director of the infectious diseases department at the University of Michigan Health-West. “For those people, COVID is still not over and so testing for early treatment is going to be critical.”
Where to get COVID tests
There are still options for getting free COVID tests around the US The last day to order four free at-home COVID tests from the government is May 31, but local community clinics can give away free COVID tests or at a lower cost until supplies run out.
Access to free testing might also depend on where you live. David Souleles, the director of the COVID-Response Team at the University of California, Irvine, says some state governments are taking measures to avoid financial barriers with COVID testing. California, for example, issued a mandate for health insurances to continue providing reimbursement for eight monthly at-home tests. Check your state government’s website to see what policies are in place following the end of the public health emergency.
If you are uninsured, the US government will continue to provide access to swabs through the Increasing Community Access to Testing Program. This government program partners with specific healthcare sites such as Walgreens and Quest Diagnostics to provide no-cost COVID tests with priority for people with a known exposure to the virus or who are showing symptoms.
[Related: An at-home test for both COVID-19 and the flu gains approval]
At-home rapid tests and PCR laboratory testing will still be available at your local pharmacies and doctor’s office, but it’s up to your insurance company if they want to bear the cost or require a copayment. What’s more, insurance companies may charge different prices for COVID tests; if they cover the cost, they may set limits on how many tests they will cover per individual.
Prices for COVID test kits in stores like CVS range from $9.99 to $28.99, meaning testing can quickly get expensive. DeHart is concerned that the prices will create a financial barrier that will deter people from getting tested. If affordability becomes a question, it’s important to make every COVID test you take count.
When it’s still important to get tested for COVID
While most COVID mandates have lifted around the country, some employers and places might require you to get tested. For instance, healthcare workers employed in facilities like nursing homes will likely continue routine COVID testing. And as of now, many hospitals still require routine COVID testing for admitted patients, though it remains unclear whether the hospitals will cover the cost or if the test will be added to a person’s medical bill.
For voluntary testing, it’s important to evaluate your risk of having a severe COVID infection. DeHart says individuals above the age of 65 and those with immunosuppressive conditions should get tested regularly, along with loved ones in close contact with those that fall under this category. Souleles also recommends taking a test before visiting a relative in assisted living or anyone who is considered at high-risk of exposure.
Other scenarios may apply, too, Souleles adds. “We would still encourage people to test before and after travel and before and after gatherings if they have the ability to do so. Anytime that you have the ability to test before you’re going to be around lots of people is great, and anytime you have the ability to test three to five days after being around a lot of people, that’s also a good thing.”
[Related: Long COVID recovery is finally getting the attention it deserves in the US]
If you have COVID-like symptoms, get tested before going out in public, even if the side effects seem mild. Testing early will give you more chances to get Paxlovid, which is most effective when taken within the first five days of seeing symptoms, and potentially avoid life-threatening complications.
If you need to purchase a COVID test, treat it like you would any other over-the-counter goods. This includes checking the expiration dates to avoid a false positive or false negative result. You will also want to throw out any recalled COVID tests. If purchased for a later date, keep COVID tests at room temperature and away from the hands of pets and young children.
What to do if you test positive for COVID
If the test comes out positive, follow the Centers for Disease Control and Prevention’s (CDC) guidelines. Stay home and isolate yourself from others in the household for five days. People experiencing moderate symptoms like difficulty breathing should isolate for 10 days. Monitor your condition and go to the hospital if there are any severe or life-threatening complications.
If you must go outside, wear a high-quality mask and avoid going to places where you would have to take it off. Also contact your doctor to see if you are eligible for any COVID-19 treatments and start those as soon as possible.
You can stop isolating after five days if you have no symptoms. If you continue to show symptoms, the CDC says you should stay put until your symptoms improve or you are fever-free for 24 hours without using medication.
[Related: Getting COVID more than once might be even worse than we thought]
Keep in mind that COVID tests are only one of the many tools available to reduce your risk of severe infection and death. Both DeHart and Souleles strongly urge people to get vaccinated and get their booster shot when eligible. Insurers will still be expected to cover the bivalent COVID vaccine as a routine immunization, and the Biden administration’s Bridge Access Program for COVID-19 Vaccines and Treatments will continue to provide vaccines free-of-charge to the uninsured.
“Stay up to date with your vaccines,” says Souleles. “It’s still the most important tool that we have right now.”