The vaccines we have today are pretty incredible. They’ve eradicated smallpox, purged rubella from the Americas, and save millions of people each year from dying of diphtheria, tetanus, whooping cough, and measles. When enough people get vaccinated, infectious diseases can’t spread easily and everyone benefits from herd immunity.
But it’s hard to reach enough people for this to happen, especially in areas with poor public health infrastructure. So scientists are taking a leaf from the virus playbook. They’re devising vaccines and antiviral therapies that can spread from host to host.
These transmissible vaccines will likely first be used in animals that carry diseases that can infect people. Some may use a weakened version of the virus, or attach a piece of the pathogen to a benign virus. Other treatments are aimed at people who are already infected and will prey on the virus dwelling in their cells.
It’s early days for these kinds of vaccines and therapies, and scientists still have to show that they are effective and safe to use in wildlife or people. But they could tamp down the spread of HIV and other contagious diseases, and immunize people who would not otherwise be protected. Plus this strategy would be cheaper than vaccinating everyone by hand.
Here are three ways we can stymie infectious diseases by spreading our own weapons.
Spreading, not quite like wildfire
There’s already at least one vaccine known to be contagious, although it wasn’t intentionally designed that way.
In the United States, the vaccine for polio is given as an injection that carries dead poliovirus. But there’s another form of the vaccine that is taken by mouth and uses a weakened—but live—version of the virus. It turns out that this version can briefly spread to other people before dying out. The World Health Organization has relied on the oral polio vaccine for its efforts to wipe out the disease worldwide.
But there is a drawback. Rarely, the live vaccine can mutate enough to revert back to its virulent form. The oral polio vaccine carries three strains of the virus, one of which has been eradicated in the wild but is also most likely to cause this problem. The WHO is switching to a vaccine that has only the two safer strains.
Vaccines signal the immune system to recognize and attack a disease-causing agent, whether they contain a virus that is alive, dead, or is only a piece of the original. This trains the immune system in case it has to encounter the real thing. Many vaccines use live but weakened versions of the virus, including those for measles and chickenpox. The process that disables the virus so it can’t cause sickness also makes it less able to spread.
But it’s likely that some of these vaccines are still a little bit transmissible. This hasn’t been studied in depth, though. When these vaccines are designed, the focus is on making sure they can’t make people sick. “Most vaccine design has not considered transmission,” James Bull, an evolutionary biologist at the University of Texas at Austin, said in an email.
If we did intentionally design transmissible vaccines, they might be more likely than regular vaccines to revert. That’s because they reach more people and have a chance to replicate and make new generations. That means more chances for mutations and evolution. “Then your transmissible vaccine turns back into the disease effectively,” says Scott Nusimer, a mathematical biologist at the University of Idaho in Moscow who has collaborated with Bull.
One way around this would be to make a live vaccine that is only weakly transmissible. This vaccine would only spread a little bit before dying out. This kind of vaccine wouldn’t be able to eradicate a disease, but fewer people would need to be directly vaccinated. A weakly transmissible vaccine would still make a major dent in disease outbreaks, Nusimer and his colleagues have calculated. “Even a little bit of transmission goes a long way,” he says.
And we would save a lot of money. If we had a transmissible version of the measles, mumps, and rubella (MMR) vaccine, we could bring down the cost of immunization by roughly $50 million per year, Nusimer estimates. “It’s astronomical the amount of money you would save, even with a weakly transmissible vaccine,” he says.
Scientists could also genetically engineer a live vaccine in ways that thwart its ability to evolve into something nasty.
Our friend, herpes
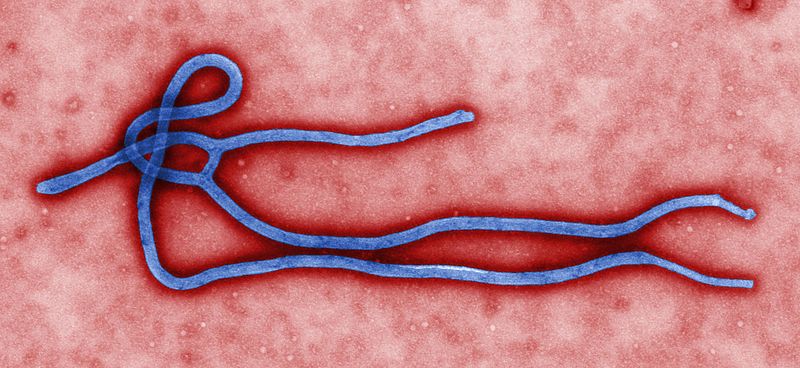
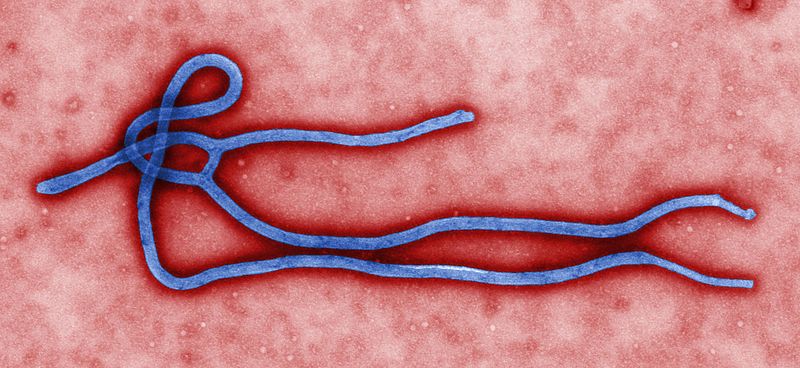
Humans are coming into closer contact with wildlife all the time thanks to construction, hunting, agriculture, and other activities that shrink natural habitats. This also means more chances for us to be exposed to the diseases they carry. About a third of Ebola outbreaks can be traced to people handling the carcasses of great apes killed by the virus, Michael Jarvis, a virologist at Plymouth University in the United Kingdom, said in an email.
So transmissible vaccines will mostly be aimed at animals that host microbes that can sicken people. This would prevent disease outbreaks in human communities and benefit endangered animals. Great apes, already in trouble because of hunting and deforestation, are also threatened by Ebola. “An ability to protect great apes by vaccination would therefore be a win-win solution for both human health and ape conservation,” Jarvis says.
It would also be much easier than trying to track down and vaccinate every ape, bat, or rodent in the vicinity. “With a traditional vaccine you’ve got to…find each individual animal and vaccinate it, which is pretty much impossible,” Nusimer says. “How do you go out there and vaccinate a bunch of deer mice against Hantavirus by hand?”
These efforts actually might not use live versions of the disease-causing virus. There’s another way of designing transmissible vaccines that is likely to prove even safer, Nusimer says. These vaccines will use benign viruses, which can infect a person or animal without making it sick. Known as cytomegaloviruses (CMV), they actually belong to the herpes family. They’re very common in both humans and other mammals. In fact, between 50 and 80 percent of adults in the United States are infected with CMV by age 40, although most have no symptoms.
In a vaccine, live cytomegaloviruses would be engineered to carry a tiny fragment of another, disease-causing virus that the immune system would recognize and attack. Should the virus revert, it would simply lose effectiveness as a vaccine. “It doesn’t have any disastrous consequences because it just goes back to being a cytomegalovirus,” Nusimer says.
These viruses can already spread easily, and many stick to just one species. So scientists could design vaccines that would limit themselves just to the kind of animals they have chosen to vaccinate.
However, the fact that they are widespread among mammals could be a double-edged sword. If the vaccine arrives in an animal that already carries CMV, it might have to compete with the normal version of the virus. So these herpes-based vaccines might not work as well as live attenuated vaccines, Nusimer says. Researchers are investigating how well multiple strains of CMV can coexist in an animal.
Jarvis and his colleagues are working on herpes-based vaccines that would immunize apes from Ebola and rats against Lassa virus. They’ve shown that their Ebola vaccine can protect macaques from the virus, although the current version is not transmissible. “The next stage is to…determine whether immunity from a self-disseminating version of the vaccine similarly provides protection,” Jarvis says. “With herpes viruses, nature and evolution has done your work for you as these viruses have evolved to spread easily.”
This kind of inoculation can also be designed not to spread. One vaccine being developed to protect humans from Ebola uses a benign virus engineered to carry a gene that codes for a protein normally found on the surface of Ebola, Nusimer says. However, that vaccine has also been stripped of the genetic instructions that enable it to replicate.
Ready to mingle
For some illnesses like HIV, there is no vaccine yet. The medicines we do have to treat HIV have come a long way in the last two decades, says Leor Weinberger, a quantitative biologist at the University of California, San Francisco and the Gladstone Institutes. “The antiretroviral therapies are a huge success story, taking HIV from what was essentially a plague to a lifelong manageable condition,” he says.
But, as with vaccines, drugs that treat contagious diseases have a few shortcomings. They can’t adapt as microbes develop resistance. “[Viruses] constantly replicate and mutate, and the chemicals that we use don’t,” Weinberger says.
And people are not always cooperative about sticking to their drugs. “Even a weeklong antibiotic regimen, people have trouble with missing a dose,” Weinberger says. And to manage HIV, people have to stay on antiretrovirals for their entire lives.
That’s why Weinberger and his colleagues are planning to give this virus a taste of its own medicine. They’re designing a debilitated, transmissible virus that, unlike a vaccine, is intended for people who are already infected. It acts as a parasite of HIV, competing with the virus for resources inside an infected cell. Weinberger calls their concoction therapeutic interfering particles, or TIPs.
To make more of itself, HIV hijacks healthy cells. These cells become factories, making the building blocks HIV needs to package its genetic material. But when TIPs arrive on the scene, they will steal these proteins for themselves. Ultimately, the cell won’t spread its contagion to its neighbors. “You’re not going to save the cell, but…what gets transmitted to the next cell is primarily the interfering particle,” Weinberger says.
By bedeviling HIV, these TIPs would lower the amount of virus circulating in a person’s blood. This should prevent them from spreading HIV to other people, and also slow the progression of HIV to full-blown AIDS.
These defective particles will be transmittable to new people. The TIPs can’t replicate without HIV, so if they spread to someone who doesn’t have HIV, they may die out. But it’s also possible that they would stick around, ready to spring into action if that person ever became infected in the future.
Because they can replicate and spawn new generations, the TIPs will also be able to evolve. They will enter an arms race with HIV so they can keep stealing from it. And should they revert back to HIV, they will simply become a virus the infected person was already carrying. “That’s like giving a drug that stops working,” Weinberger says.
There are other safety concerns that he and his colleagues must still address. “We have to make sure that we defang it in a way that it’s actually defanged [and] that it won’t revert back to something worse than the original,” Weinberger says. They also have to make sure the TIPs can’t cause an overactive immune response that would make a person sicker.
They are still perfecting the TIP design and will test them in animals for the next year or two to make sure they are safe. The team has focused on HIV, but a similar strategy could be used for other viruses, Weinberger says.
